Trauma Isn’t Everything—But It Is Part of Being Human
In recent years, trauma has become one of the most common lenses through which we understand mental health. The idea that “trauma is everything” has entered popular culture, therapy spaces, and social media alike. On the one hand, this shift has been profoundly important. Experiences that were once minimized or dismissed are now being taken seriously. People are finally finding language for pain that lived silently in their bodies for years.
And yet, somewhere along the way, the conversation has tipped into something that feels…off.
If everything is trauma, then what does that say about us as humans? Are we truly that fragile? Do we really need to live our lives constantly scanning for triggers, managing ourselves as though we might break at any moment?
I don’t think so.
Trauma as an Experience, Not an Identity
I do believe this: any overwhelming experience can be encoded in the body as trauma. The nervous system doesn’t judge severity the way the mind does. What overwhelms one person may not overwhelm another, and that’s okay. Trauma isn’t a moral category—it’s a physiological and emotional response.
But acknowledging that trauma can arise from many experiences doesn’t mean we need to organize our entire identities around it.
When trauma becomes the primary story we tell about ourselves or our clients, something important gets lost. We start to see people not as adaptive, creative, resilient beings—but as perpetually injured. Healing becomes framed as endless management rather than natural integration. Life starts to feel like a minefield instead of a landscape.
That’s not liberation. That’s another kind of constraint.
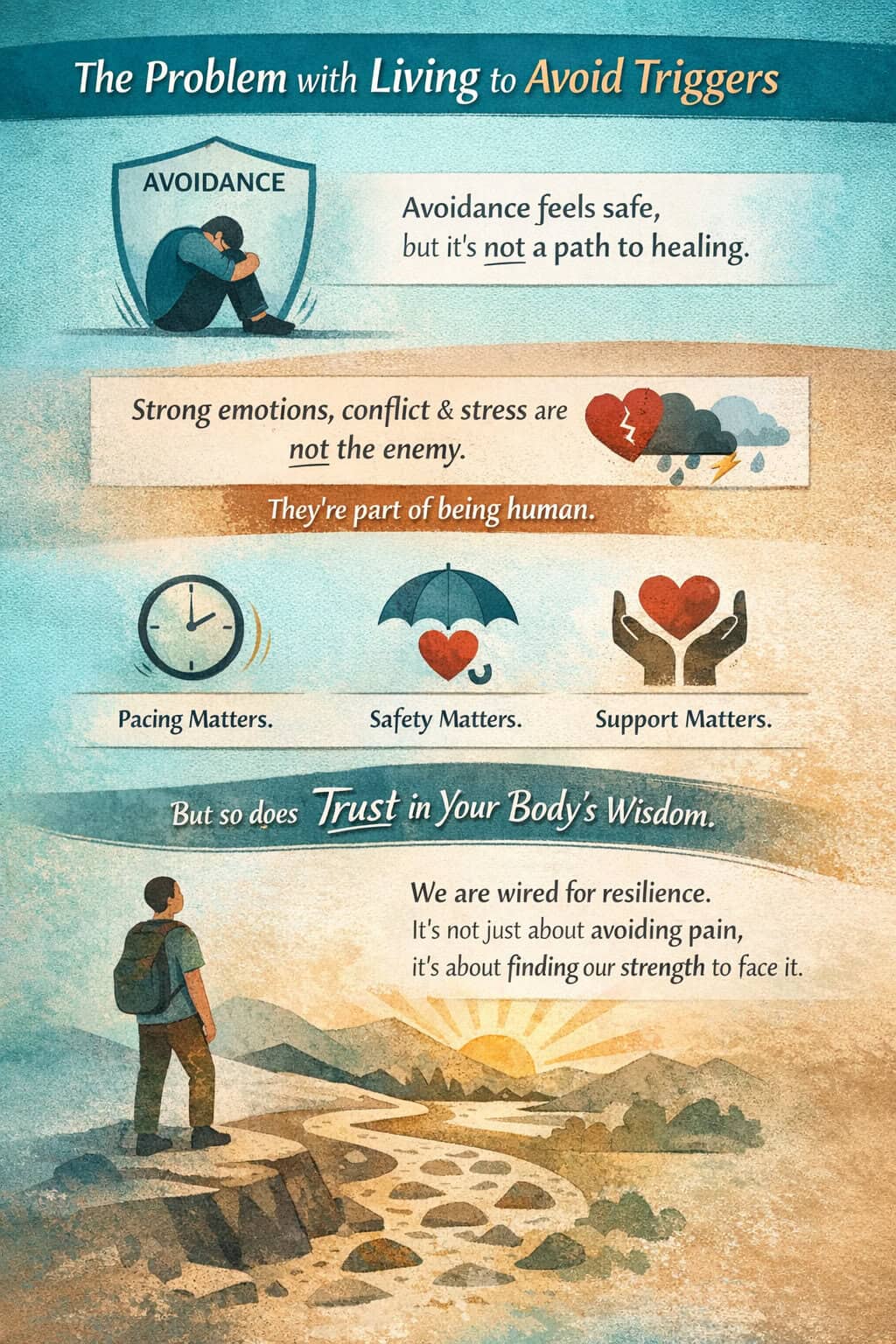
The Problem With Living to Avoid Triggers
There’s a subtle but powerful message embedded in a trauma-obsessed culture: You are safest when you avoid discomfort.
But avoidance has never been a path to healing.
If we orient our lives around preventing activation at all costs, we teach the nervous system that it can’t handle intensity. We unintentionally reinforce the belief that strong emotions, conflict, grief, or stress are dangerous rather than meaningful.
Yes, pacing matters. Safety matters. Support matters. But so does trust—especially trust in the body’s innate capacity to move through experience.
Humans have been encountering loss, fear, rupture, and uncertainty for as long as we’ve existed. What’s different now is not the presence of hardship, but the story we tell about our ability to survive it.
Trauma Doesn’t Have to Be “Other”
One of the unintended consequences of modern trauma discourse is that trauma gets treated as something separate from ordinary human life—something abnormal, exceptional, or defining.
But what if trauma isn’t “other” at all?
What if it’s simply one of many ways the nervous system responds to intensity?
Seen this way, trauma isn’t evidence of weakness. It’s evidence of impact. And recovery isn’t about erasing what happened—it’s about restoring movement, choice, and connection.
When trauma is normalized as part of the human experience, shame softens. People don’t feel broken for having symptoms. And at the same time, they don’t feel doomed to carry those symptoms forever.
The Body Knows How to Heal
One of the most overlooked truths in mental health is this: the human body and spirit inherently know how to heal.
We see this everywhere. Cuts close. Bones knit. Grief moves. Emotions crest and fall. Even intense nervous system responses are designed to resolve—when they’re met with enough support, time, and permission to complete their cycle.
Healing isn’t something we impose from the outside. It’s something we facilitate by removing obstacles and restoring conditions that allow the system to do what it already knows how to do.
We are not machines in need of constant correction.
We are organisms designed for adaptation.
Resilience and Growth Are Not Rare
Post-traumatic growth is often spoken about as though it’s an exception—a lucky outcome for a few resilient individuals.
In reality, growth after adversity is common. Not inevitable, not forced—but accessible.
People frequently report greater clarity, deeper compassion, stronger boundaries, and more meaningful relationships after surviving difficult experiences. This doesn’t mean trauma was “good” or necessary. It means humans are capable of integrating pain into wisdom.
When therapy focuses only on minimizing symptoms without honoring growth, we miss an essential part of the healing arc.
A More Empowering Frame
What if therapy didn’t position clients as fragile systems to be protected from life, but as capable systems learning to trust themselves again?
What if we held trauma with seriousness and faith in recovery?
This doesn’t mean rushing healing or bypassing pain. It means remembering that safety and strength are not opposites. That vulnerability and resilience coexist. That being affected by life does not make someone broken—it makes them human.
Trauma matters. It deserves attention, compassion, and skillful care.
But it doesn’t have to be everything.
And neither do you.
Ready to get started?
At The Catalyst Center, we support people in exploring trauma with depth, care, and trust in their innate capacity to heal. If you’re curious about therapy or ketamine-assisted psychotherapy as a way to reconnect with resilience and wholeness, we’re here to walk alongside you.